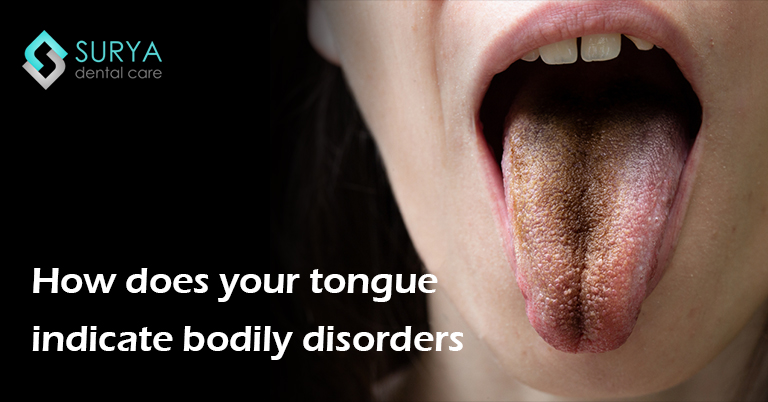
White tongue is a medical condition that is used to describe any part of the tongue that has a greyish white coating. This coating can occur in patches or the entire tongue could be coated. There are many reasons that can cause a white tongue and each cause has a separate treatment. So it’s important to know the specific cause to find a cure. Although most time, a white tongue is usually harmless but sometimes it could indicate a serious medical condition that should be treated immediately.
Pale Tongue (Anemic Appearance)
A pale or “ghostly” tongue is often a sign of anemia (low red blood cells) or iron‑vitamin B deficiency. The tongue may appear uniformly light pink or white‑ish, feeling smooth due to atrophy of papillae. Other symptoms include fatigue, dizziness, brittle nails, and pale skin. Diagnosis can be confirmed with a simple blood test. Treatment focuses on correcting nutritional deficiencies—iron, B12, folate—through diet or supplements, and monitoring with your healthcare provider. With proper care, the tongue often returns to a healthy pink tone within weeks.
Causes
There are different causes of white tongue. An overgrowth and swelling of papillae which looks like fingerlike projections is caused by residual food particles, bacteria and dead cells that gets lodged between the ridges of the tongue and inflamed papillae.
Some of the causes of papillae inflammation include, for example:
- Poor oral hygiene
- Dry mouth
- Dehydration
- Smoking or or tobacco use
- Excessive alcohol
- Mouth breathing
- Low roughage diet (eating mostly soft or mashed foods)
- Fever
Some other causes include
Oral lichen planus
An inflammatory condition affecting the mouth, it causes white patches of skin to appear in the tongue and parts of the mouth. These white patches could appear alone or alongside different symptoms. Some of those symptoms include ulcers, pain in the cheeks and gums etc.
Leukoplakia
Leukoplakia forms thick white patches on the tongue and mouth. It can either be caused by the use of tobacco and alcohol or due to irritation caused by wearing dentures. Mostly the patches that leukoplakia causes are harmless but in rare cases can have serious complications. Therefore it is advisable to visit a doctor for diagnosis.
Oral Thrush
Another condition that may cause tongue to appear white is oral thrush. Caused by a specific form of yeast called ‘Candida yeast’, it causes patches to develop in the mouth and on the tongue. This condition can also be painful, especially when eating or drinking.
COVID‑19 & White Tongue
During the COVID‑19 pandemic, many patients reported transient white tongue or coated tongue as part of COVID‑19‑associated oral manifestations. This is believed to stem from changes in oral microbiota and dehydration. While the coating usually resolves as the infection and hydration improve, persistent or painful coatings should be evaluated by a dentist or medical practitioner, especially if accompanied by other systemic symptoms.
Syphilis
Syphilis is a sexually transmitted infection that can cause sores in your mouth. If syphilis isn’t treated, white can form on your tongue.
Some other conditions that may cause white tongue include:
- Geographic tongue that look like islands on a map
- Some antibiotic medicines can cause a yeast infection in your mouth
- Mouth or tongue cancer
Treatment
Good oral care can help in the removal of white tongue. Some common treatment practises are:
- Using a soft toothbrush when brushing the teeth.
- Using a mild toothpaste
- Brushing or scraping the tongue
- Using a straw to drink cold drinks.
- Avoiding spicy, salty, acidic things as well as moderating consumption of alcohol and cigarettes
- Food and drinks that are very hot in temperature.
- Take over-the-counter painkillers
- Stay well‑hydrated—COVID and other infections worsen oral coatings
- Boost nutrition (iron, B12, folate) when tongue looks ‘pale’
- Probiotics or antibacterial mouth rinses may help restore healthy tongue flora.
Treatment for serious diseases:
- Leukoplakia: Visit the dentist if the white patch does not go away on its own after around two weeks. Completely discontinue the usage of alcohol and tobacco.
- Oral lichen planus: This can last for several years so a visit to the doctor is recommended. Maintaining good oral hygiene is key to reducing oral pain.
- Geographic tongue: Should go away on its own but needs to keep a note of the diet. Avoid food and drinks that are known to increase discomfort.
- Oral thrush: Some antifungal medications are recommended by the dentist which should be applied to the patches inside the mouth. This type of treatment can last a few weeks.
- Syphilis: Syphilis is a sexually transmitted diseases and is quite serious. It should be treated as soon as the symptoms are diagnosed or it could cause long-term health issues by damaging the nervous system and attacking the brain.
when to see a professional
If the coating persists beyond two weeks despite proper hydration, hygiene, or supplementation—especially if painful, patchy, or accompanied by fever, weight loss, oral sores, or systemic signs—consult your dentist or doctor promptly to rule out underlying infections or nutritional conditions.
FAQs
It may indicate benign causes (bacterial buildup, dehydration) or conditions like oral thrush, leukoplakia, lichen planus. Sometimes, a pale tongue suggests anemia. Rarely, it could signal systemic or infectious diseases. Persistent white patches warrant professional assessment.
Generally, no. Most causes—poor oral hygiene, dehydration, medications, or oral thrush—aren’t sexually transmitted. However, some STIs like syphilis can present oral lesions. If you suspect an STI, seek medical evaluation immediately.
Maintain strict oral hygiene: brush and scrape your tongue daily, rinse with salt water, stay hydrated, avoid tobacco/spicy and acidic foods. If due to thrush or nutritional deficiency, follow your dentist's advice for antifungals or supplements.
















Leave a Comment